Dry Eye Syndrome: When Your Eyes Feel Parched (and a Warm Hug Makes it Better)
- What is Dry Eye Syndrome?
- What Causes Dry Eye Syndrome?
- Diagnosing Dry Eye Syndrome
- Treating Dry Eye Syndrome: Finding Relief
- Additional Tips for Managing Dry Eyes
- Differential Diagnosis of Dry Eye Symptoms
- Potential Complications of Untreated Dry Eye
- When to See an Eye Care Professional (Ophthalmologist/Optometrist)
- References
What is Dry Eye Syndrome?
Do you frequently experience sensations like grittiness, burning, or persistent dryness in your eyes? If these feelings are familiar, you might be among the millions of individuals affected by Dry Eye Syndrome (DES), also known as keratoconjunctivitis sicca. This common and often chronic condition can be incredibly frustrating, impacting daily activities and overall comfort. The good news is that numerous effective treatment options are available, ranging from simple home remedies like artificial tears to therapeutic interventions such as the comforting warmth of a heated eye mask.
Understanding Tear Film Dysfunction
Dry Eye Syndrome occurs when your eyes either do not produce an adequate quantity of tears (aqueous-deficient dry eye) or when the tears produced are of poor quality and evaporate too quickly (evaporative dry eye). A healthy tear film is essential for maintaining the health of the front surface of the eye and for providing clear vision. It consists of three layers:
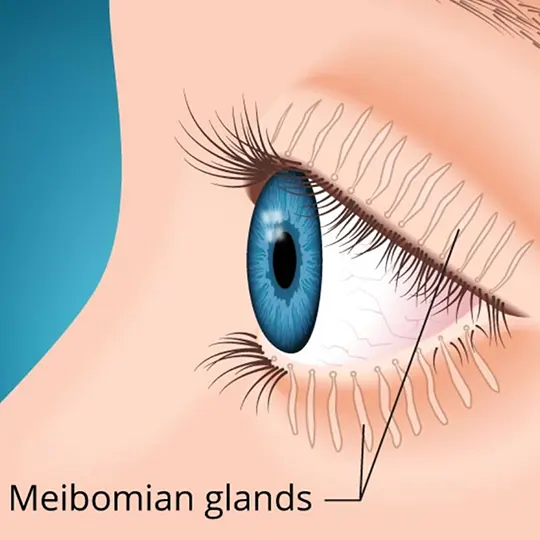
- The Oily (Lipid) Layer: The outermost layer, produced by the meibomian glands in the eyelids. It smooths the tear surface and reduces evaporation of the watery layer.
- The Watery (Aqueous) Layer: The middle and thickest layer, produced by the lacrimal glands. It lubricates the eye, washes away debris, and provides essential nutrients and oxygen to the cornea.
- The Mucus (Mucin) Layer: The innermost layer, produced by goblet cells in the conjunctiva. It helps the tear film spread evenly over the surface of the eye and helps the tears adhere to the cornea.
An imbalance or deficiency in any of these layers can lead to tear film instability and the symptoms of dry eye.
Common Symptoms of Dry Eye
The symptoms of Dry Eye Syndrome can vary in intensity and may include:
- A stinging, burning, or scratchy sensation in the eyes.
- A feeling of grittiness or having something in the eye.
- Stringy mucus in or around the eyes.
- Eye redness and irritation.
- Sensitivity to light (photophobia).
- Blurred vision, especially when reading or after prolonged screen use, which may temporarily improve with blinking.
- Eye fatigue, particularly after concentrating for long periods.
- Difficulty wearing contact lenses comfortably.
- Paradoxically, periods of excessive tearing (watery eyes). This can occur because the dryness irritates the eye surface, triggering a reflex production of a large volume of poor-quality tears that don't lubricate effectively.
What Causes Dry Eye Syndrome?
There are many potential factors and conditions that can contribute to the development of Dry Eye Syndrome. These can be broadly categorized into those causing decreased tear production and those leading to increased tear evaporation.
Decreased Tear Production (Aqueous-Deficient Dry Eye)
- Aging: Tear production naturally tends to decrease with age. Dry eye is more common in older adults, particularly women after menopause due to hormonal changes.
- Medical Conditions:
- Autoimmune Diseases: Sjögren's syndrome is a classic example, directly affecting tear and saliva glands. Other conditions like rheumatoid arthritis, lupus (Systemic Lupus Erythematosus), scleroderma, and thyroid disorders can also be associated with dry eyes.
- Diabetes.
- Vitamin A deficiency (rare in developed countries).
- Medications: Many common medications can reduce tear production as a side effect, including:
- Antihistamines and decongestants.
- Certain antidepressants and anti-anxiety medications (e.g., tricyclic antidepressants, SSRIs).
- Blood pressure medications (e.g., diuretics, beta-blockers).
- Hormone replacement therapy or oral contraceptives.
- Acne medications (e.g., isotretinoin).
- Parkinson's disease medications.
- Lacrimal Gland Damage: Damage to the tear-producing glands from inflammation, radiation, or injury.
- Corneal Nerve Desensitivity: Reduced corneal sensation (e.g., after long-term contact lens wear, LASIK surgery, or due to conditions like herpes zoster ophthalmicus or diabetes) can decrease the reflex tearing mechanism.
Increased Tear Evaporation (Evaporative Dry Eye)
This is the most common form of dry eye and often relates to issues with the meibomian glands.
- Meibomian Gland Dysfunction (MGD): The meibomian glands, located in the eyelids, produce the oily layer of the tear film. If these glands become blocked or inflamed (blepharitis), they don't secrete enough oil, leading to rapid tear evaporation. Congealed oils can build up and clog the tear ducts (orifices) of these glands.
- Environmental Factors:
- Dry air (low humidity), windy conditions, or exposure to smoke.
- Indoor environments with heating or air conditioning.
- High altitudes.
- Reduced Blink Rate: Prolonged staring at computer screens, smartphones, or while reading can significantly reduce the blink rate, leading to increased tear evaporation.
- Eyelid Problems: Conditions like ectropion (eyelids turn outward) or entropion (eyelids turn inward) can affect proper tear spreading and eyelid closure. Incomplete eyelid closure during sleep (nocturnal lagophthalmos).
- Contact Lens Wear: Can disrupt the tear film and increase evaporation.
- Vitamin A Deficiency: Can affect goblet cell function, reducing mucin production necessary for tear film stability.
Diagnosing Dry Eye Syndrome
An eye care professional (ophthalmologist or optometrist) can diagnose Dry Eye Syndrome based on:
- Patient History: Discussion of symptoms, medical history, medications, and environmental factors.
- Comprehensive Eye Examination:
- Visual Acuity Test.
- Slit-Lamp Examination: To examine the eyelids, conjunctiva, cornea, and tear film. Special dyes like fluorescein or lissamine green may be used to highlight areas of dryness or damage on the ocular surface.
- Tear Break-Up Time (TBUT): Measures how quickly the tear film evaporates after a blink. A short TBUT indicates tear film instability.
- Schirmer's Test: Measures the volume of aqueous tear production by placing small filter paper strips inside the lower eyelids for a few minutes.
- Meibomian Gland Evaluation: Assessing the function and oil quality from the meibomian glands.
- Tear Osmolarity Test: Measures the salt concentration in the tears; higher osmolarity is often found in dry eye.
- Questionnaires: Standardized questionnaires (e.g., Ocular Surface Disease Index - OSDI) can help quantify symptom severity.
Treating Dry Eye Syndrome: Finding Relief
The good news is that a variety of effective treatments are available for Dry Eye Syndrome. The best approach for an individual will depend on the type of dry eye (aqueous-deficient or evaporative), the severity of symptoms, and the underlying cause. Treatment often involves a stepwise approach, starting with simpler measures.
Artificial Tears and Lubricants
Over-the-counter artificial tears are typically the first line of defense for most people with mild to moderate dry eye. These products help to lubricate the eyes, supplement the natural tear film, and relieve symptoms. They come in various formulations:
- Preservative-Free Drops: Recommended for frequent use (more than 4-6 times a day) or for individuals sensitive to preservatives, as preservatives can sometimes irritate the eyes with long-term use.
- Drops with Preservatives: Suitable for less frequent use.
- Gels and Ointments: Thicker formulations that provide longer-lasting lubrication, often used at bedtime as they can temporarily blur vision.
- Lipid-Containing Eye Drops: Specifically designed to help restore the oily layer of the tear film, beneficial for evaporative dry eye due to MGD.
Prescription Medications
If artificial tears are not sufficient, an eye doctor may prescribe medications:
- Cyclosporine (e.g., Restasis®, Cequa™): An immunomodulator that helps to reduce inflammation associated with chronic dry eye and can increase natural tear production over time.
- Lifitegrast (e.g., Xiidra®): Another anti-inflammatory medication that targets specific pathways involved in dry eye disease.
- Corticosteroid Eye Drops: Short-term use of steroid drops can quickly reduce severe inflammation but are generally not for long-term management due to potential side effects (e.g., increased eye pressure, cataracts).
- Autologous Serum Eye Drops: Made from the patient's own blood, these drops contain growth factors and nutrients beneficial for severe dry eye and ocular surface disease.
- Nasal Sprays for Tear Production (e.g., varenicline nasal spray - Tyrvaya®): Stimulates a nerve pathway to increase basal tear production.
In-Office Procedures
- Punctal Plugs: These tiny, biocompatible inserts are placed into the tear ducts (puncta) in the corners of the eyelids. They block tear drainage, thereby keeping natural and artificial tears on the eye surface longer. Plugs can be temporary (dissolvable) or permanent (silicone).
- Meibomian Gland Expression/Procedures: For MGD, procedures like LipiFlow®, TearCare®, iLUX®, or manual gland expression can help to unblock meibomian glands and improve oil secretion.
- Intense Pulsed Light (IPL) Therapy: Used to treat inflammation associated with MGD and rosacea.
- Amniotic Membrane Grafts: For severe ocular surface damage.
Lifestyle Changes and Home Remedies
Making some simple changes to daily habits and environment can significantly help improve dry eye symptoms:
- Use a Humidifier: Especially in dry indoor environments (e.g., during winter with heating or in arid climates) to add moisture to the air.
- Avoid Dry Air and Wind: Protect eyes from direct drafts from fans, air conditioners, or car vents. Wear wraparound sunglasses outdoors to shield eyes from wind and sun.
- Take Breaks from Screens: Follow the "20-20-20 rule": every 20 minutes, look at something 20 feet away for at least 20 seconds. Consciously blink more often when using digital devices. Position screens below eye level.
- Dietary Considerations: Consuming a healthy diet rich in omega-3 fatty acids (found in fatty fish like salmon, flaxseeds, walnuts) may help improve tear quality and reduce inflammation. Omega-3 supplements may be beneficial for some.
- Stay Hydrated: Drinking plenty of water is important for overall health, including tear production.
- Eyelid Hygiene: For MGD or blepharitis, regular gentle cleaning of the eyelid margins with a mild cleanser or specialized eyelid wipes can help remove debris and bacteria, and keep meibomian gland openings clear.
Heated Eye Masks: A Warm Embrace for Your Eyes
Applying gentle, consistent heat to the eyelids using a heated eye mask can be a wonderfully soothing and highly effective home treatment for managing dry eye symptoms, particularly those related to Meibomian Gland Dysfunction (MGD).
How Heated Eye Masks Work
The therapeutic warmth from a heated eye mask provides several benefits:
- Melts Clogged Meibomian Gland Oils: The meibomian glands produce an oily substance (meibum) that forms the lipid layer of the tear film, preventing rapid tear evaporation. In MGD, this oil can become thickened or congealed, blocking the gland openings. Heat helps to liquefy these solidified oils, allowing them to flow more freely and improving the quality of the tear film.
- Stimulates Tear Production: While primarily aiding the oil layer, the warmth can also generally soothe the eyes and may indirectly support overall tear function.
- Improves Eye Circulation: Gentle heat can increase blood flow to the eyelid area, which may promote gland health.
- Provides Comfort and Relaxation: The warmth itself is often very soothing for irritated, tired eyes.
Choosing and Using a Heated Eye Mask
- Types of Masks: Options range from simple microwaveable masks filled with flaxseed or beads, to electric USB-powered masks, to specialized medical-grade devices.
- Temperature and Duration: Look for masks that provide a gentle, consistent warmth (typically around 40-45°C or 104-113°F) for about 5-15 minutes per session. Masks with adjustable temperature settings can be beneficial. It's important that the mask warms the meibomian glands to the therapeutic temperature needed to melt congealed oils.
- Hygiene: Choose a mask with a washable cover or one that can be easily cleaned to maintain hygiene.
- Frequency: Use as directed by your eye care professional, often once or twice daily for MGD.
- Safety: Always follow the manufacturer's instructions. Ensure the mask is not too hot to avoid burns. Test the temperature on your wrist before applying to the eyes. Do not use if you have certain eye conditions or recent eye surgery without consulting your doctor.
Remember, you're not alone! Millions of people live with Dry Eye Syndrome, and there are many resources and treatments available to help you manage your condition effectively. With the right combination of professional advice and self-care strategies, including the cozy comfort of a heated eye mask when appropriate, you can find significant relief from your symptoms and enjoy a better quality of life.
Additional Tips for Managing Dry Eyes
Beyond the primary treatments, these simple habits can further help:
- Avoid Rubbing Your Eyes: This can worsen irritation and potentially introduce bacteria.
- Blink Regularly: Especially during prolonged visual tasks like computer work or reading, make a conscious effort to blink fully and frequently to help spread tears evenly.
- Protect Eyes from Wind and Sun: Wear wraparound sunglasses or goggles in windy conditions or bright sunlight.
- Review Medications: Discuss with your doctor if any of your current medications could be contributing to dry eye symptoms; alternatives may be available.
- Cool Compresses (for discomfort): While warm compresses/heated masks are primarily for MGD, applying a cool compress to closed eyelids can sometimes help soothe acute discomfort, itching, or swelling associated with general eye irritation.
Differential Diagnosis of Dry Eye Symptoms
Symptoms like burning, grittiness, and redness are common to many eye conditions. It's important to differentiate Dry Eye Syndrome from other possibilities:
| Condition | Key Differentiating Features |
|---|---|
| Dry Eye Syndrome (DES) | Burning, grittiness, foreign body sensation, blurred vision (improves with blink), light sensitivity. Positive diagnostic tests (TBUT, Schirmer's, staining). |
| Allergic Conjunctivitis | Itching is a predominant symptom; watery discharge, redness, eyelid swelling. Often seasonal or related to allergen exposure. |
| Bacterial or Viral Conjunctivitis (Pink Eye) | Redness, discharge (purulent in bacterial, watery in viral), eyelid crusting, foreign body sensation. Often contagious. |
| Blepharitis | Inflammation of the eyelid margins; redness, crusting, flaking at the base of eyelashes, itching, burning. Often coexists with MGD and DES. |
| Corneal Abrasion or Foreign Body | Sudden onset of severe pain, foreign body sensation, tearing, photophobia, redness. History of trauma or exposure. |
| Contact Lens-Related Issues | Discomfort, redness, dryness specifically related to contact lens wear; possible overwear, poor fit, or solution sensitivity. |
| Computer Vision Syndrome (Digital Eye Strain) | Eye strain, headaches, blurred vision, dry eyes, neck/shoulder pain associated with prolonged screen use. Symptoms often improve with breaks. |
| Sjögren's Syndrome or other Autoimmune Diseases | Severe dry eyes and dry mouth, may have other systemic symptoms (joint pain, fatigue). Specific autoantibodies may be present. |
Potential Complications of Untreated Dry Eye
If Dry Eye Syndrome is left untreated or is severe, it can lead to complications:
- Corneal Damage: Chronic dryness can lead to abrasions, erosions, infections (keratitis), ulceration, and even scarring of the cornea, potentially affecting vision.
- Increased Eye Infections: The tear film helps protect the eye surface from infection. Reduced or poor-quality tears can increase susceptibility.
- Decreased Quality of Life: Persistent discomfort, blurred vision, and light sensitivity can significantly impact daily activities like reading, driving, working on a computer, and overall well-being.
- Difficulty with Contact Lenses: Many people with dry eye find it difficult or impossible to wear contact lenses comfortably.
When to See an Eye Care Professional (Ophthalmologist/Optometrist)
It is important to consult an eye care professional if you experience persistent or worsening dry eye symptoms, especially if:
- Over-the-counter artificial tears do not provide adequate relief.
- Symptoms are severe and interfere with your daily life.
- You experience eye pain, significant redness, or changes in vision.
- You have a known medical condition that can cause dry eyes (e.g., Sjögren's syndrome, rheumatoid arthritis).
- You are unsure about the cause of your symptoms.
An eye doctor can perform a comprehensive examination to diagnose Dry Eye Syndrome, determine its underlying cause and type, and recommend an appropriate, individualized treatment plan.
References
- The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007 Apr;5(2):75-92.
- Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017 Jul;15(3):276-283.
- Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017 Jul;15(3):334-365.
- Jones L, Downie LE, Korb D, et al. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017 Jul;15(3):575-628.
- Bron AJ, Tiffany JM, Gouveia SM, Yokoi N, Voon LW. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004 Mar;78(3):347-60.
- Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1922-9.
- American Academy of Ophthalmology Cornea/External Disease Panel. Preferred Practice Pattern® Guidelines. Dry Eye Syndrome. San Francisco, CA: American Academy of Ophthalmology; 2018. (Refer to latest version).
- Blackie CA, Korb DR, Knop E, et al. Nonobvious Meibomian Gland Dysfunction. Cornea. 2010 Dec;29(12):1333-45.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal